2022 UoA Physiotherapy Programme
The University of Auckland, my 'alma-mater' that I attended in NZ in the 1980's, had asked for volunteers to visit their Newmarket campus for sessions.
''…neurological physiotherapy course. I would like to bring in people with stroke to work with the students so that they can practice an interview and assessment as they learn so much more quickly working this way rather than practicing on each other. It would be about 1.5 hrs at 2:30 on a Monday in Newmarket. ..”
Cool - definitely interested when I am back in Auckland... I was in Penang Malaysia, on family matters when the email arrived from the University lecturer leading the programme.
Back now in Auckland, the date was set was for the appointment; it had been some years since I did my last session with the University of Auckland. For quite some years for post-stroke it involved volunteering participation for quite some years for post-stroke Physiotherapy for walking studies with PhD candidates, participating in Speech-after-stroke research project's post-graduate study, etc... It's rewarding to be involved in research to find solutions and aids, or help train new therapists with hands-on approach so others don't have to go through what I had to back in 1995.
We arrived at the Newmarket campus with plenty of time to spare. This was my first time at this new campus – in my university days it was a brewery owned/occupied by Lion Breweries; times have changed significantly.
The gym I was led to was bright, light, cavernous and full of equipment; a big space, reminiscent of the gym in London* hospital where I spent three months in 1995, after my massive AVM-haemorrhage, thence stroke. *where my husband Murray and I were on our OE (overseas experience) journey.
In London, a team of neurosurgeons performed emergency open-brain surgery which took 9 hours - Murray was pacing the floor, in an agonising wait. That was after the seven hours delay from the time I fell unconscious at work (was an IT professional) and when my colleagues called the ambulance. I was admitted to the nearest hospital, but they couldn't deal with such an extreme neurological case so I had to be taken to the second hospital in central London to accept me as an emergency case.
[And… 6 months later, another procedure was done: Linear accelerator Stereotactic radiosurgery for arteriovenous malformations (AVM) to treat the remainder left within my brain.]
...I led a healthy life. Didn't smoke; didn't drink to excess; ballroom-danced; skied at Whakapapa and Queenstown in NZ, then Bulgaria and Austria when in Europe; exercised, even running up and down stairways in my high heels instead of using lifts, every day.
We travelled extensively, to sometimes quite exotic world destinations every chance we had in our time in the Europe... – what on earth could have happened?
Happy and lively one moment, .. when I woke up post-surgery I found that I couldn't: stand or walk; talk; read; write; remember; lying prone in a hospital bed, I couldn't move at will anymore, right-side paralysed, in a wheelchair later on. I had serious clonus and footdrop, sub-lux shoulder, severe aphasia....and the list goes on. Having to Relearn Life from scratch was only the beginning of the journey; I was 34 years old. (see: STROKE, life after AVM article)
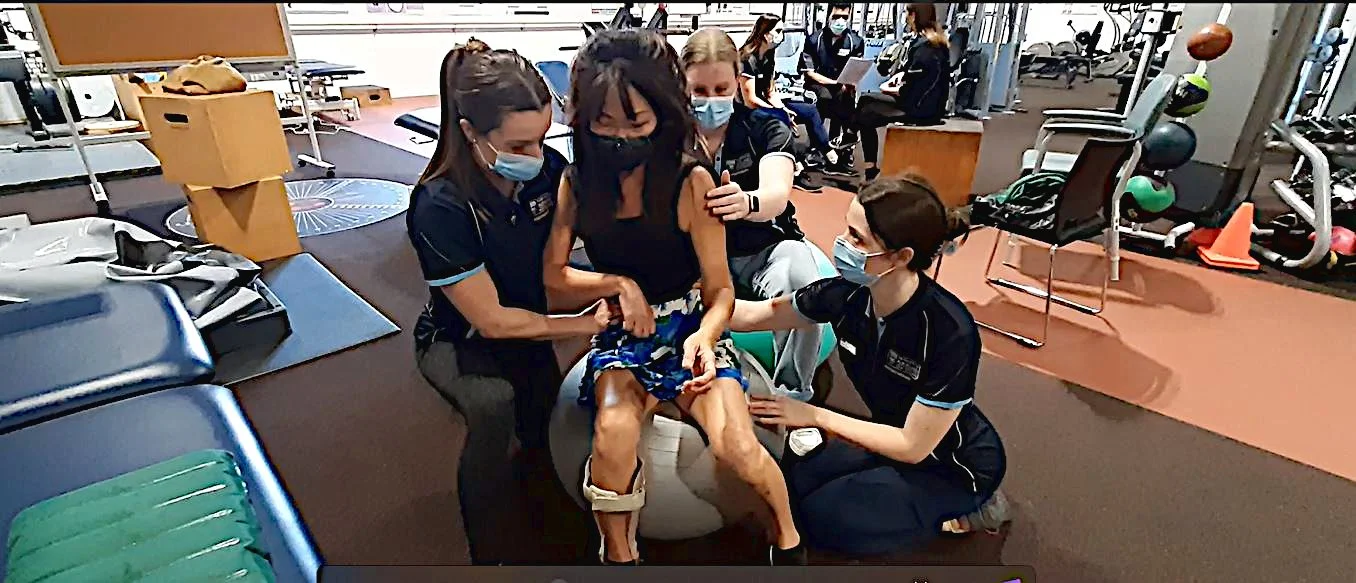
Reminiscing over, we got underway very quickly; the students were already practising. The students are post-graduate, and this is the first time to practice on real people who've had strokes rather than practice on themselves, before clinical placements. Learning skills to become physiotherapists in a 2-year Masters of Physiotherapy course.
It was informative for me, and very instructive for the students - each team had different skills to master, where they rotated the roles and took turns to practice the steps; I was involved with 3 groups. The lecturer demonstrated the movements of the activity. The correct way for the student to guide and support, holding the patient (me) firmly yet allowing me to try and do the activity, is the key to the exercise.
From an activity-list the students had, the next exercise was to sit on a …what were the names again: balance, Physio, space hopper, or fitness ball...? I knew them from the hospital in London; remembered that I really dreaded the experience. Back then, I had very little (in fact no) balance at all in hospital in central London.
Post-stroke, nurses had to do everything for me – I couldn't turn in bed, so I had to sleep facing up each night. My left side was unaffected, but to do anything the whole body needed to coalesce and work together – my right side was so extremely heavy after the stroke, I couldn't hold my body upright for too long, even when I was in a wheelchair later on; like an unbearable weight was suddenly put on me after the stroke.
Stand...you must be kidding me.., really? Muscles in my right leg weren't driven by brain impulses, so now I had to try to will them to work – it was excruciatingly painful to stand, even three seconds was too long in the legacy wooden standing-frame in hospital.
A challenge in the hospital in London in the use of the fitness-ball: .. was that I couldn't readily talk to Physiotherapist (hadn't the 'words' to describe my concerns, as I had to learn English again after the stroke) - that I was almightily afraid of falling for whatever reason - .. the 'ball' just didn't look that safe for me to sit on. As I couldn't remember even very short sentences (short-memory was totally blitzed), for years, Murray and I had to play charades-for-real as I would forget what I was about to say two words into the very-slurred sentence, day in day out.
Back to the present and the fitness ball: the student therapists were ready to support me if I was to feel unsafe, to catch me before I fell off, in the extreme case. Rolling/side-to-side my control of the ball exercise, still not the best but I've come a long way since London, so that was pretty good.
Sitting up, lying down on a plinth, standing; some exercises were using the balance/fitness ball. At times the activities were challenging, but others were surprisingly okay. All in all, I now don't feel as wary of the fitness-ball as I did before.
The other sets-of-movement that surprised me was my ball (the size of a basketball) handling skills. I was seated, as was student therapist – he threw a ball at me, I was supposed to catch it. I was a right-hander before my AVM-stroke, and a netballer at school. Now, only my left hand usable, I have very little movement on the right – how would I fare?
Tossing the ball to and fro at different heights – I'm one-handed,.. I caught most balls. Tossing rings or small-hoops, ..left or right, which direction, I wondered? - there was a 50% chance (was my initial thought) either way, judge height from the ground, speed of the ball or hoop... and lunge and catch-it at the correct cue? If only it were that easy... - ...I've had 27 years of trying to do activities one-handedly, hmm..
... not having played netball in a very long time, perhaps brain plasticity had something to do training the mind again to work out problems and would-be solutions on the go; delving on my past examples and playing it out via a different tune, with left/right hand? Exercises and activities with other modalities I was involved through stroke-rehab and brain plasticity over the past few years, perhaps focussed my mind a bit more – an interesting thought. See: Walk research with EEG and FES article and Video.
To 'walk' is automatic, what able-bodied persons do without much thought. Walking on loose-sandy beaches, down to the waterline where one sinks in ever so slightly; polished surfaces or glass floors; skateboarders, scooters and cyclists careening very close, …: to keep balance: change stance, side-step them, do whatever was called for in my pre-stroke days.
Now, I walk with a marked gait,.. - a challenge to know how to move, if you have great sensory impairments and/or loss – it is not automatic any more, I've found. Besides my right-side being very stiff and tight, I have to remember to move my weight at the correct time, keep the right posture and refrain from hip-hitch. On an incline or down some ramps, to watch where I'm going just in case anyone brushes close and upsets my balance - dips & bumps and choices in the chosen path do matter now in everyday walking.
Millions of possibilities, to ponder the situation before it arises, is perhaps a good thing. The student therapists practicing exercises and activities on us participants, also provided an illuminating session for me, to listen and try to emulate (on myself when I practice my walk...).
We had a rushed time in Penang (my hometown) on family affairs, at the start of the article - if we had the chance of a couple of hours to spare, great opportunities to look around Georgetown, Pearl of the Orient as is sometimes known as, also a UNESCO world heritage city.
Penang: one of the renowned Street-food capitals of Southeast Asia, in travel columns, magazines, Lonely Planet articles - impressive heritage and blending of cultures, balmy beaches - remain mouth-wateringly fabulous.
Many thanks to:
Marie-Claire Smith PhD, NZRP , Lecturer
Auckland Medical Research Foundation Research Fellow
Department of Exercise Sciences / Te Kura Mātai Kori Tinana, Faculty of Science
University of Auckland
...also Best Wishes to the team of post-graduate Physiotherapy student therapists 2022.